|
|
||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||
|
http://emergency.cdc.gov/coca/summaries/COCA-UnsafeInjectionPractices.asp
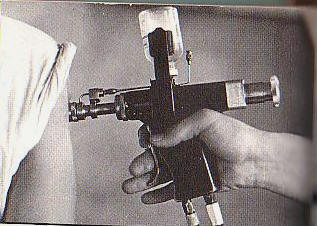
Transcript: COCA Conference Call Ė A ďNeverĒ Event: Unsafe Injection Practices (March 27, 2008)NOTE: This document is provided for historical purposes only and may not provide our most accurate and up-to-date information. The most current Clinician's information can be found on the Clinician Home Page. COCA Conference Call Ė A ďNeverĒ Event: Unsafe Injection Practices Coordinator: Welcome and thank you for standing by. At this time all participants are in a listen-only mode. To ask a question during the question and answer session please press Star 1 on your touchtone phone. Todayís conference is being recorded, if you have any objections you may disconnect at this time. I would like to turn the meeting over to your host for todayís conference, Miss Alycia Downs; Maíam, you may begin. Alycia Downs: Thank you. Good afternoon and thank you for joining us for todayís COCA conference call entitled A ďNeverĒ Event: Unsafe Injection Practices. We are very pleased to have Doctors, Perz, Srinivasan and Patel present on this call. We will be using a PowerPoint presentation that you should be able to access on our Web site. If you have not already downloaded this presentation, please go to www.emergency.cdc.gov/coca; click on the conference call information Summaries and Slide Sets, the PowerPoint can be found there. All of our speakers today work in the Division of Healthcare Quality Promotion in the National Center for Preparedness, Detection and Control of Infectious Diseases here at the Centers for Disease Control and Prevention. Dr. Perz is an Epidemiologist on the Prevention Team in the Prevention and Response Branch. Dr. Patel is a Medical Epidemiologist in the Prevention and Evaluation Branch. And Dr. Srinivasan is the Team Leader for the Response Team. Our objectives for this call: after this activity the participants will be able to: -Describe safe injection and other basic infection control practices and be able to recognize and correct unsafe practices. -They should be able to understand the need for monitoring healthcare personnel practices in your facility relating to injection safety and basic infection control. -Describe the potential consequences of syringe reuse and other unsafe practices, and -Locate related CDC infection control guidance and educational materials. In compliance with continuing education requirements all presenters must disclose any financial or other relationships with the manufacturers of commercial products, suppliers of commercial services or commercial supporters as well as any use of unlabeled products or products under investigational use. CDC, our planners and the presenters for the seminar do not have financial or other relationships with the manufacturers of commercial products, suppliers of commercial services or commercial supporters. This presentation does not involve the unlabeled use of a product or products under investigational use. I will now turn the call over to Dr. Perz. Joseph Perz: Thank you everyone for joining this discussion of a very important patient safety issue. Unsafe injection practices represent breakdowns in basic infection control during the preparation and administration of parenteral medications. Iím turning now to Slide 3, which shows headlines from 2001 and that these headlines make clear the topic has generated a great deal of attention in recent years Ė next slide Ė attention which continues to the present. Hereís a headline from the New York Newsday from this past December. Concern has grown as these types of incidents continue to accumulate most recently in NY City, Michigan, Long Island, New York and Las Vegas, Nevada. Next slide. Miss Downs has already reviewed the learning objectives. I just would like to add that we do feel itís critical that we in public health along with healthcare providers and our other partners work together to tackle this problem head on. Next slide. Letís review an outline of the presentation. First weíll review an example of what we mean by a ďNeverĒ Event. And weíll discuss an important concept, that of indirect transmission. Then weíll talk about injection safety, define that and give some examples of unsafe practices. Then weíll review recommendations and strategies aimed at the prevention of disease transmission from unsafe injections. Weíll present some frequently asked questions and a summary. And then if time remains, open up the line for questions and answers. Next slide. Probably the best example of a ďNeverĒ event related to injection safety and breakdowns in basic infection control, in my mind, is that of the Nebraska hepatitis C outbreak, which affected cancer patients. And though it was reported in the Annals of Internal Medicine that article is freely available and I encourage you to look at it if you have time. Letís delve into some of the details then of that outbreak. In September 2002 four patients who were recently diagnosed with hepatitis C virus or HCV infection were reported to the Nebraska Health Department. The clinician who saw these patients and made the diagnosis noted that they had one thing in common, which was that they had all regularly received chemotherapy at one clinic. The initial investigation by the health department identified infection control breaches related to catheter flushing. And this prompted the notification of over 600 patients who were considered to have been at risk during an 18-month period. In the end, 99 clinic-acquired HCV infections were identified. And we have likened this to 99 wrong side surgeries occurring in one setting; it was really a stunning example of what can go wrong. These infections were all with a single unusual genotype of HCV, which is genotype 3a, and the transmission period was defined as March 2000 to July 2001. Next slide. So what actually went wrong? Well as the first bullet shows, here the nurse who was in charge of providing chemotherapy infusions would draw blood from these patientsí indwelling IV catheters, remembering that these are cancer patients who are coming back for regular infusions of chemotherapy and most of them had indwelling IV catheters. The nurse would check the patency of that catheter by drawing some blood back into the syringe, discharging it, changing the needle and then Ė using the same syringe to access a 500cc bag of saline Ė actually performed the flush. A new syringe was used for each patient so this is not overt reuse of a syringe from one patient to the next. Nonetheless contamination of this large bag of saline could expose many, many patients to infection. The clinic was located in or near a hospital but was actually independently owned and operated and did not have an active infection control program. Breaches had been identified during the time the transmission occurred but were never reported to the state health department and were not corrected until June of 2002. In 2004 the oncologistís and registered nurseís license were revoked. This is Ė this actually represents a growing concern in that CDC and state and local health departments have since this time investigated an increasing number of outbreaks related to unsafe injection practices as well as other breaches in very basic infection control. And the trend is concerning in that detection of transmission of this type can be haphazard. Just using the hepatitis viruses as an example, acute or new infections are often asymptomatic and do not come to the attention of medical providers. And also thereís a low index of suspicion because we trust that healthcare in our country is safe; thereís Ė itís sometimes hard to make the connection back to those healthcare exposures. Consider too that hepatitis C and some of the other infections that weíll talk about have a long incubation period. Outbreaks are occurring across the spectrum of healthcare in the US. And examples include ambulatory care, home care, long-term care settings and as we know these are settings where unlike hospitals, formal infection control infrastructure programs and oversight are often lacking. Another example of a tragic outbreak affecting vulnerable cancer patients is the one that Iím showing here on Slide [12], an outbreak of catheter associated Klebsiella and Enterobacter bloodstream infections Ė this time in a cancer clinic in Chicago. This was investigated in 2004 and reported in the Archives of Internal Medicine in 2005. The outbreak also involved improper flush procedures Ė weíll come back to this in a minute Ė and unfortunately resulted in 27 cancer patients hospitalized with bloodstream infections. And as the accompanying editorial makes clear, History Forgotten is History Relived, itís a reminder that infection control and the infrastructure that we associate with hospitals is also essential in the outpatient setting. Letís take a few minutes to review some basics in terms of transmission of infections. Turning to Slide [14]. Indirect contact transmission refers to the transfer of an infectious agent through a contaminated intermediate object or person. And examples of this include the hands of healthcare personnel, patient care devices (an example being glucometers), instruments (an example being endoscopes that are not adequately reprocessed being patient uses), and medications and injection equipment. And thatís further illustrated on the next slide. You may have to advance twice so that you should now be seeing a slide with a yellow title, Transmission of Pathogens Via Contaminated Equipment or Medication and a yellow figure on the left and a white figure on the right. And so what weíre showing here, in simple visual terms, is the idea that two patients who may never actually come into direct contact with one another can actually be part of a chain of transmission. If the source patient who has a particular infection of interest comes into contact with equipment that is then shared with a second case, transmission can occur if that equipment Ė whether it be a finger stick device, glucometers, endoscope, syringe, needle or medication vial Ė if that has become contaminated and remains contaminated when the next person is exposed to that equipment or medication, infection can occur. Next slide. This slide is a way of illustrating this for a ubiquitous procedure, that being a finger stick blood draw to test blood glucose level. It illustrates I think nicely how, you see, if infection control practices arenít followed carefully, blood from that patientís finger can either remain on the healthcare workers hands, for example, if gloves arenít changed, or it can contaminate the device. And note that a study by the University of California in Davis several years ago showed that over 30% of glucometers in hospital studies had detectable blood contamination on them. And weíve seen a number of hepatitis B outbreaks in the long-term care settings in connection with either the reuse of a finger stick device from patient to patient or failures to clean glucometers and other breakdowns in basic infection control. The next slide shows an injection preparation table. Weíre not singling out Pakistan, this is a condition which unfortunately we could find in many healthcare settings around the world in which we see open multi-dose medication vials on one side of the table and used injection equipment on the other side and a lot of potential for either blood contamination to carry over and expose the next patient or for bacterial growth to occur. Moving on then. What is injection safety? Injection safety includes practices intended to prevent transmission of infectious diseases between one patient and another or between the patient and healthcare provider and also to prevent harm such as needle stick injuries. Recognizing that the exposure and infection risks to healthcare workers are fairly well understood at this point weíll be focusing on the risk to patients in this talk. Another way to define safe injection is that a safe injection does not harm the recipient nor does it expose the provider to any avoidable risks and does not result in waste that is dangerous for the community. And as I said, in the US risks to providers remain and are of concern and weíll talk a bit about that here but for the most part weíre going to focus on risks for patient-to-patient spread today. So the next slide. What are some of the incorrect practices that have resulted in transmission of pathogens? Well, using the same syringe to administer medication to more than one patient, in other words, direct reuse of the syringe from one patient to the other even if the needle was changed is one example. Using a common bag of saline or other IV fluid for more than one patient. And leaving an IV set in place for dispensing fluid as was observed in the Chicago outbreak that I described earlier, the Klebsiella and Enterobacter bloodstream infection. Or, to access the bag of saline or shared container with a syringe thatís already been used as was described in my review of the Nebraska outbreak. And finally something thatís similar to the accessing of a saline bag with a syringe thatís been used, accessing any shared medication vial with a syringe thatís already been used to administer medication to a patient. And weíll work through that on the following slide which is an illustration that we are borrowing from the Southern Nevada Health District developed in connection with the recent outbreak of hepatitis C virus associated with . . . an endoscopy clinic in Las Vegas. And the point of this is just to show that we can begin an injection procedure with a clean needle and syringe and a new vial, draw medication from that syringe, from that vial, administer it using the syringe and if the patient is infected with a blood borne virus, in this case HCV or hepatitis C virus, there is the potential for backflow of blood or virus into the syringe. If that particular patient then requires additional anesthesia using that same vial, if that vial is used to withdraw the additional medication, even if the needle is changed, blood can be introduced or virus can be introduced into what was a clean vial. If that vial is then used for a subsequent patient even using, at that point, a clean needle and a clean syringe, that patient Ė or subsequent patients Ė exposed to that vial are placed at risk. Next slide. So to summarize some of the points that weíre reviewing. Unsafe injection practices do put patients at risk for a wide variety of adverse events and have been associated with a wide variety of procedures. Examples include administration of anesthetics for outpatient surgical, diagnostic and pain management procedures, the administration of other IV medications including chemotherapy, cosmetic procedures and alternative medicine, examples being chelation therapy or injections of vitamins or steroids, next, flushing IV lines or catheters and in some cases administration of intramuscular vaccines inappropriately. So turning to the next slide, weíll review with the following examples, the broad range of settings, procedures and adverse outcomes associated with unsafe injection practices. So hereís an example of cosmetic procedures leading to adverse events, in this case skin reactions in the District of Columbia in 2005. This lad us to publish an MMWR article where we reiterated some of the infection control and safe injection practices that we have over the past years increasingly felt the need to transmit and to educate providers about. Be aware that this problem in terms of unsafe cosmetic injections continues and there were recent reports for example from North Carolina of patients with kidney failure following unsafe cosmetic injection. Moving on. Hereís an example of the transmission of a parasite, malaria, associated with improper use of saline flush syringes. This occurred in a hospital environment between two patients who shared a room and the apparent mode of transmission was the inadvertent reuse of a prefilled saline syringe. The next slide illustrates that in fact HIV has also been transmitted through unsafe injection practices. This example is taken from Denmark from Copenhagen and transmission was attributed to the mishandling of multi-dose vials. Next slide shows four outbreaks reported in the MMWR in 2003. And this collection of outbreaks was something of a wake-up call for us in the US that in fact this problem of unsafe injection practices which we didnít always associate with US healthcare, you know, in fact could be a problem here as well as in the developing world. So weíll run through some of these examples. The first one was an endoscopy clinic in New York City in 2001 in which 19 HCV infections were identified in the course of an investigation and transmission was attributed to the contamination of the multi-dose anesthetic vials. And the next slide just shows again how this is something which, you see, affects us in many ways including adverse attention, letís say, to healthcare, which is a concern given the importance of maintaining patient trust in healthcare in preventive and other services. Moving on then. The next slide shows the Oklahoma Pain Remediation Clinic outbreak also reported in that MMWR. And hereís an example of overt reuse of a syringe from one patient to the other can transmit infection. Weíll go through it quickly but weíll point out that this outbreak was not detected until six patients with acute hepatitis C were diagnosed. All had received treatment at a single pain clinic and the clinician who noted that then reported that to the health department. This was an outpatient clinic but was affiliated with a hospital. Anesthesia staff were contractors. And this pain clinic was operated just one afternoon per week. A nurse anesthetist working in this facility had been reported for poor practice but unfortunately the first report was not acted upon by managers and the second report in June 2002 did result in a formal reprimand and change in practice. But the department of health was not notified; at that time the disease transmission had not been recognized. The next slide shows in a little bit more detail what happened. The anesthetist had the routine practice of filling a single syringe with sedation medication in quantity sufficient to treat all the patients they would see that afternoon. And this medication was administered through heparin locks. Subsequently the anesthetist, upon interview, indicated that,it was his perception that he had a sterile field given that there was a length of IV tubing and the heparin lock. The look back investigation for the entire two-year time period of clinic operation ended up having to notify over 900 patients, nearly 800 had serologic results available. Seventy-one of these had clinic associated hepatitis C virus infections, 31 had clinic associated HBV infections, several patients unfortunately acquired both infections. And one outcome of this was a very large lawsuit. And the next slide shows a billboard that, you know, always gives us pause. We think about how, you know, being in public health of course and doing, you know, surveillance for these viruses and other infections, but this is not something that youíd want to see across from your clinic obviously. Moving on to the New York City outbreak, 2001. Two patients both elderly, not your typical patients in terms of acute hepatitis B, were in fact diagnosed with acute hepatitis B. Theyíd been admitted to the same hospital and attended the same private medical practice. The clinician who noticed this reported it to the New York City Health Department and with CDC an investigation ensued. This resulted ultimately in the notification of over 1000 patients, over 200 of whom had test results available. They identified almost 40 patients with acute hepatitis B virus infection. The Ė moving ahead to the last bullet, what was happening here was that infection was associated in our epidemiological studies with injections of vitamins and steroids, two or three medications actually mixed together in one syringe. And the next slide reviews some of the common themes and findings from those outbreaks and also applies to outbreaks that have occurred in the interim. First of all investigations are resource intensive and disruptive to patients and providers and to the public health system. And just one example is that these investigations often require the notification, testing and counseling of hundreds and even thousands of patients. We also realized in those outbreaks from the MMWR report, delayed recognition and missed opportunities to intervene. Transmission occurred over a prolonged period and in some of these outpatient settings with patients returning for recurring care, for example for chemotherapy or in the previous example patients were coming back every couple of weeks for the vitamin shots. We see then a growing reservoir of infected patients and the potential for a large outbreak. We also note that, again, infection control programs are lacking or responsibility is unclear in many of these outbreak facilities. And again this is entirely preventable by applying standard precautions and basic principles of aseptic technique. So turning now to some of our prevention messages. Letís move on to the next slide. Consider that injection safety and basic infection control are all part of very basic patient safety. Healthcare should not provide any avenue for transmission of blood borne viruses. And when thatís recognized it shows a breakdown in basic patient safety and should be treated as a red flag or sentinel event. We also would like to see the risks of patient-to-patient spread better recognized and put on par with, you know, the recognition and intolerance of risks for blood borne pathogens to be transmitted to healthcare workers or through blood transfusion. And as I said this is entirely preventable. [Ö] Again, Standard Precautions and aseptic technique can keep this from happening. I also would like to draw attention on the next slide to an important document published last year. It is the Guideline for Isolation Precaution: Preventing Transmission of Infectious Agents in Healthcare Settings. This is a publication of CDCís Healthcare Infection Control Practices Advisory Committee. One reason Iím trying to draw your attention to this is as is shown on the next slide and as is stated in the Executive Summary, the recognition that the transition of healthcare delivery, as we discussed earlier, from primarily acute care hospitals to other settings, ambulatory care being an important one, made it important to make clear that, you know, these guidelines and standard precautions, which is the foundation for preventing transmission of infectious agents, that clearly this has to be applied in all healthcare settings. And in particular the outbreaks of hepatitis B and hepatitis C virus in ambulatory settings indicated a need to reiterate safe injection practice recommendations clearly as part of standard precautions. And you see a link there below to the full document. The next slide is difficult to read and we wonít go through it in detail at this point except, again, to draw your attention to the fact that within standard precautions there are just this set of safe injection practice recommendations. And weíll, on the following slide, touch on some that we would like to highlight. So moving to the next slide, here are just some selected examples of safe injection practices: One, to always use aseptic technique to avoid contamination of sterile injection equipment. Next, use single dose or single use vials for parenteral medications whenever possible. Next, needles, cannulae and syringes are sterile single use items that should not be reused for another patient nor to access a medication or solution that might be used for a subsequent patient; and to not use bags or bottles of IV solution as a common source of supply for multiple patients. The next slide weíll talk a little bit more about aseptic technique which is the handling, preparation and storage of medications and all supplies used for injections and infusions in this context, syringes, needles, IV tubing, in a manner that prevents microbial contamination. Medications should be drawn up in a designated clean medication preparation area. And in general any item that could have come in contact with blood or body fluids should be kept separate from that area. The next slide illustrates the fact that injection preparation on surfaces where contaminated substances are handled can lead to the spread of infections. And this picture was actually taken from the New York City outbreak that involved the injection of vitamins and steroids. And as you see the limited space available to prepare injections in this preparation room included the storage of multi-dose vials and preparation of injections in the same area that used needles and syringes were actually dismantled and discarded. Next slide. Safe Handling of Parenteral Medications, to review some important principles here; one, the necessity of always using a new sterile syringe and needle to draw up medications. Next proper hand hygiene should be performed before handling medications. And that parenteral medications and injection equipment should be accessed in an aseptic manner. In the next slide we discuss the importance of maintaining the sterility of vials and the recommended practices. A new sterile needle and syringe should be used for each injection. Medications should be discarded upon expiration or any time there are concerns regarding the sterility of the medication. Leftover parenteral medications from single use vials in particular should never be pooled for later administration. And a needle or other device should never be left inserted into a medication vial septum for multiple uses as this provides a direct route for microorganisms to enter the vial. Next slide. An important principle in terms of adding in a layer of patient safety is that of minimizing the use of shared medication as this reduces patient risk. Single use vials, for example, propofol, should never be used for more than one patient. Multi-dose vials should be assigned to a single patient whenever possible. And in general the number of patients sharing a vial should be limited. Do not use bags or bottles of intravenous solution as a common source of supply for more than one patient. And again maintaining absolute adherence to proper infection control practices must be maintained during the preparation and administration of injected medications. Itís also important, as the next slide illustrates, to develop a culture of safety. And one way to do that is through administrative measures. So it is recommended that:
And at this point weíre going to move on and present some frequently asked questions. And Iím going to ask my colleagues Dr. Patel and Dr. Srinivasan to help us with that. Priti Patel: One frequently asked question is if it is acceptable to use the same syringe to give intramuscular or IM or subcutaneous injections to more than one patient if the needle is changed in between patients. The answer is no, once they are used the syringe and needle are both contaminated and must be discarded. A new sterile syringe and needle should always be used for each patient. Arjun Srinivasan: The next question is one that has come up a lot and deals with a common misperception about the issue of changing the needle only. Is it okay to use the same syringe to give an IM or IV injection to more than one patient if I change the needle between patients and I donít draw back before injecting? And the answer to that is no; there is a small amount of blood that can flow into the needle and the syringe even when only positive pressure is applied Ė even if you donít draw back. Which means that in every situation the syringe and needle should both be considered contaminated and must be discarded. Priti Patel: And a related question is: If I use the syringe only to infuse medication into an IV tubing port that is several feet away from the patientís IV catheter site, is it okay to use the same syringe for another patient? And the answer is no; everything from the medication bag to the patientís IV catheter is a single interconnected unit. An important point that is often confused, separation from the patientís IV by distance, gravity and/or positive infusion pressure does not ensure that small amounts of blood are not present in these supplies. A syringe that intersects through ports and IV tubing or bag also becomes contaminated and cannot be used for another patient. Arjun Srinivasan: Another question thatís come up a lot particularly with the recent publicity of the episode in Nevada; are these recommendations new? And I think this is, again, an important point to emphasize that the answer is no, these recommendations are definitely not new; theyíre parts of established guidance. Itís a well established practice to never use the same syringe or needle for more than one patient. And not to enter a medication vial with a syringe or needle used for one patient if that vial is going to be used for another patient. Priti Patel: And for the question, how can healthcare providers ensure that injections are performed correctly? We recommend the following: designate someone to provide ongoing oversight for infection control issues, develop written infection control policies, provide trainings in infection control and conduct quality assurance assessment. Arjun Srinivasan: The next question is I think an important one because it has been one thatís lead to some degree of confusion. Can I reuse a syringe during a procedure for a patient who requires additional medication as long as the vial will not be used for another patient? And technically this may be an acceptable practice; it does not pose a risk of pathogen transmission as long as that vial is never used for another patient. But to provide an additional margin of safety we do believe that itís preferable to use a new sterile syringe to withdraw medications even if youíre only going to use it for one patient. Priti Patel: And finally comes the issue of visual inspection. And the question is, why canít I just visually inspect syringes to determine whether or not they are contaminated or can be used again? The answer is that pathogens including hepatitis C virus, hepatitis B virus and human immunodeficiency virus or HIV can be present and in sufficient quantities to produce infection in the absence of visible blood. Similarly bacteria and other microbes can also be present without clouding or other visible evidence of contamination. So just because you donít see blood or other material in a used syringe or IV tubing or both it does not mean that the item is free from potentially infectious agents. All used injection supplies and materials are potentially contaminated and should be discarded. Joseph Perz: [Ö] As we reviewed, improper use of syringes, needles and medication vials can result in, one, transmission of life threatening infections to patients; two, notification of patients of possible exposure to blood borne pathogens and recommendations that they be tested for hepatitis C virus, hepatitis B virus and human immunodeficiency virus and three, referral of providers to licensing boards for disciplinary action has occurred in several of these instances and malpractice suits have been filed by patients. So some key take-home messages. All healthcare providers are urged to carefully review their infection control practices and the practices of all staff under their supervision. And in particular providers should never administer medications from the same syringe to more than one patient even if the needle is changed. And second, never enter a vial with a syringe or needle that has been used for a patient if the same medication vial might be used for another patient. And with that Iíd like to draw your attention to links to some CDC materials that weíve developed. And that we hope you will help us disseminate to the members of your professional groups or to your fellow practitioners. And these include, as youíll see, both summary of the messages that were presented here in the form of something that could adapt itself to a letter or material for a newsletter as well as a more complete list of frequently asked questions. So with that we thank you very much for listening and want to point out that you may send us your questions, thoughts and concerns using the telephone number or the email address listed there as well as the email address for the Clinician Outreach [and Communication] Activity. Alycia Downs: Thank you very much, that was a very informative presentation. So we can now go ahead and open up the lines for the question and answer session. Coordinator: Thank you. At this time we are ready to begin the question and answer session. If youíd like to ask a question you may press Star 1, you will be prompted to record your name. Please unmute your phone and record your first and last name. Once again if youíd like to ask a question you may press Star 1. Our first question, you may ask your question. Question: Hi. I actually wanted to share an experience that I had with my youngest son in an emergency room. They used a needleless system there and my son was afraid of the needleless system. And the nurse decided to place the needleless system on his hair along his arm. And then wanted to proceed to inject my son and I had to stop him. Not only is it, you know, a supervisorís responsibility to stop infection breaches but itís all of our responsibilities who know better. Take the time when you see infection breaches to stop the person, educate them on how to do better. And if they need further review then, you know, guide them or report that to a supervisor because that could cause a significant Staph infection on anybody who, you know, decides to rub needle along their hair and inject into someoneís arm. Joseph Perz: Well thank you. Thatís a very good point and one that, you know, I think we should all take to heart that itís all of our responsibilities. Speak up when needed. Coordinator: Thank you. Our next question. Question: Hi. My concern is with large flu clinics where Iíve seen and actually done it myself with multiple dose vials; itís hard to set up an area where you have a clean area for drawing up the medication and then move across to your patient when you have lots of patients coming. So what does the CDC recommend specifically with large flu clinics vaccinations? Joseph Perz: I would say that -- in that setting, as in any other setting -- it is important to set up properly and to do what it takes to make sure that you have a clean preparation area that has some separation from surfaces that might be contaminated. Arjun Srinivasan: Yeah, I think a point thatís been raised by people in this setting is that there doesnít have to be a tremendous geographic distance between the areas there just needs to be a very clear demarcation of the clean and dirty areas. So it can be accomplished in a fairly confined space with some clever use of proper ways to really demarcate the clean and dirty areas. Joseph Perz: And I would add one more thing which is that we realize that there are often time pressures connected with healthcare delivery. And, you know, the busy flu vaccine clinic might be one example. But I think weíd all agree that there are certain compromises that we should not make. Coordinator: Thank you. Our next question. Question: Hi. Thank you very much for a very clear and timely presentation. I had a couple of questions and one is a follow up to the question about flu vaccinations. You mentioned on Slide [21] Ė or you have listed on Slide [21] administration of IM vaccines as a possible route for transmission of pathogens. Do you have Ė you didnít go into examples of vaccines causing transmission of infectious agents. Do you have examples of those either handy or on your Web site? Joseph Perz: Well thanks for bringing that up. And that is more of an example of something that can go wrong but where we donít have actual evidence of transmission in US healthcare settings. For example, in Ė on Long Island, New York last year there was a lot of publicity surrounding a large notification. And I think one of the slides Ė one of the early slides actually showed a cover of a newspaper regarding that. And the publicity surrounding that actually prompted a report from somebody working in an OB/Gyn clinic. And they actually recognized unsafe practice in their setting as a result of that publicity. And so there was an example of a clinic where they had been drawing up multiple doses of flu vaccine into a syringe and then changing the needle between administrations. So we realize that unsafe practices do sometimes occur in the context of delivery of IM injections for vaccine. And so itís worth drawing attention to. Question Contíd: Absolutely. And did that get written up in peer review literature are you aware or? Joseph Perz: You know, there are media reports surrounding that. However, we have not at this point published that formally. Question Contíd: And one other quick question for you. On one of your last slides, Slide [57] you provide the link to a CDC Web page. I was able to look at the slides a little bit earlier today and tried that link out several times and canít get the page to work. So I thought I would just mention that to you and maybe you could, a little bit later, look at that again and make sure weíve got the proper link. Joseph Perz: Okay, well it was our goal to have that link live by the time of the call. SoÖ Question Contíd: Oh I see. Joseph Perz: Yeah. Question Contíd: I will try it again then in a little bit. Joseph Perz: Okay. Coordinator: Thank you. Our next question; you may ask your question. Question: I have two questions. One is about to swab or not to swab with an alcohol swab. And the second is my particular need is for basic resources on aseptic technique for the purpose of teaching medical assistants in regard to immunization. And so I donít know, you know, if the CDC Web site Ė I tried that link also, itís not working now. I donít know if the CDC Web site will have that type of really basic thing but if not do you have any particular resources to recommend for that? Thank you. Priti Patel: So to clarify the first part of the question, you mentioned alcohol swab, are you referring toÖ Question Contíd: On vials. Priti Patel: The medication vial. And we do say that if a medication vial has been opened previously and has been entered that it should be swabbed with alcohol swabs prior to entering it again. Question contíd: And how about if itís a brand new single use and you just opened it? Priti Patel: It certainly doesnít hurt to swab it with an alcohol swab. Question Contíd: Okay. Priti Patel: Your second question was about resources for, specifically, medical assistants in terms ofÖ Question Contíd: Yes, kind of basic, you know, at a pretty basic level about aseptic techniques. Priti Patel: Thatís not something that we have targeted our resources towards. But I think some of the materials that will be on our Web site will hopefully be helpful. Question Contíd: Thank you. Coordinator: Thank you. Our next question, your line is open. Question: Could you speak to the issue of sharing glucometers between nursing home residents whereas the lancet is changed but the glucometer is not sanitized between each resident? Joseph Perz: Unfortunately outbreaks erlated to that practice occur and are identified by state health departments and reported to CDC with some regularity. And what we see is that they Ė about half of the outbreaks are associated with a finger stick device, like for example a spring-loaded lancing device thatís actually used from patient to patient, which is something that CDC and FDA have recommended against for over 15 years. And yet that practice persists. And so we are working with partners in those areas to, you know, make sure that that message is out there. However, as you point out, that risk can persist even when a safety lancet is used for every patient. And, you know, I alluded to it in the talk; those glucometers are often not cleaned between patient uses. And blood contamination is often evident; itís often visibly evident and then, as well, we have at least the one study from UC Davis, you know, showing a high frequency of contamination of those devices. And if thereís blood on the device, even if the healthcare provider performs appropriate hand hygiene, changes gloves between patients, in handling the glucometers they may then introduce Ė they may have blood or virus introduced to their gloves and expose a patient that way. So CDC does have specific recommendations around safe blood sampling. Much of that was summarized in the MMWR article in 2005. Question Contíd: Thank you. Coordinator: Next question, your line is open. Question: This is Ė I had a question just basically, I guess itís general, but having gone to school in the 60s and like you said earlier none of this is new, I mean, I learned all of what you talked about today regarding the disposable syringes and needles, you know, 40 years ago. So where do you think the breakdown is, is it in you know, really the educational system or are there just rogue providers out there who think they, you know, they basically have better solutions to financial solutions? Arjun Srinivasan: I donít know that anybody knows definitively whatís going on. Youíre absolutely right; itís something thatís not novel, itís been known. We suspect itís a variety of issues that some people maybe arenít as well educated as they need to be. We also, though, acknowledge that, you know, some of this can be viewed to some of the pressures that are put on providers these days to see more patients, to see them more quickly, to save money wherever possible. So you have in some ways and in some of those settings kind of a perfect storm for adverse events to happen. If you read the patient safety literature any time you create those types of pressures there can be problems. Question Contíd: So ethics takes a back seat and you go for the dollar I guess? Arjun Srinivasan: I think thatís a definite concern. So I think that itís both a potential knowledge deficient and a potential cutting corners issue. And obviously both of those have to be addressed equally. Joseph Perz: Yeah, and Iíll also add that, you know, CDC is pursuing strategies that involve having more basic infection control training as part of oneís training before entering the healthcare profession Ė as well as strategies around, for example, accreditation and continuing education. Question Contíd: Thank you. Coordinator: Next question. Question: Thank you. My question is with respect to retractable syringes. The instructions ask that the needle be retracted while still in the patient. In my experience sometimes it doesnít happen while itís still in the patient; itís hard to deploy. Is it safer to then put the entire syringe in the sharps container? My experience is that it sprays a little when you do it outside the patient; thereís a spring that forces the fluid out. Have there been any studies on the safe use of retractable syringes? Joseph Perz: Well, -- the use of safety devices in that context -- which can enhance provider protection is an important issue and one thatís received a lot of attention. Iím not familiar with a specific recommendation regarding the practice that you described in terms of activating the device, you know, that if itís not possible to do it, while the needle is still in the patient. Iím afraid that I donít have a specific guidance on that. But if you email or write us weíll do our best to get back to you. Question Contíd: Thank you. Coordinator: Next question. Question: Hi. Thank you very much for putting together this excellent presentation. We really appreciate it. Iíve got a question about the use of a single syringe and needle even on the same patient. And I would include with this question the use of a multi-dose vial or a single dose vial from which multiple doses may be withdrawn even for the same patient. The question Ė one of the comments that you had made on here in a couple of different places including in the FAQs is that while itís not absolutely wrong to reuse a syringe and needle on the same patient or withdraw from a vial as long as that vial is not going to be used for other patients. It has been our understanding that when you pull back on the plunger of a syringe the plunger itself is contaminated. And once you then inject the medication the inside of the barrel is then considered contaminated. And even on the same patient you canít draw back new medication and administer it to the same patient because that syringe is contaminated. And not just with the patientís own infectious disease, process, whatever is going on, but from whatever is on the practitionerís hands or if the syringe happened to be laying on a table that was contaminated. And so Iím not sure I understand why you would say that we could reuse the needles and a used needle and syringe on the same patient. In addition, from the universal precautions, any time we use a contaminated syringe or needle to try to refill it to give to a patient the user increases the likelihood that they could stick themselves with a contaminated needle. And I just was wondering if you had considered that and what your thoughts are on that? Joseph Perz: Thank you. Priti Patel: Thank you for those questions. I think from our standpoint we are trying to highlight practices that have been implicated in terms of patient-to-patient transmission of blood borne pathogens. And so thatís where we focused our messages. But we agree that the best practice is to never reuse a syringe even on the same patient. Question Contíd: In that case then I would like to ask if you would consider changing some of the areas on the slides so that it reflects that it just not as a preferred but that a single use syringe and needle should never be reused even on the same patient because you could be contaminating the patient with something that you picked up on your hands from somebody you just shook hands with and contaminating them. So you are transferring from patient to patient itís just through a different mechanism and also exposing the provider. Joseph Perz: Thatís a very good point. Weíll follow up on that. And I think thatís an example of where this type of dialogue with providers does help inform recommendations and make them more useable. Question Contíd: And I Ė the reason I bring this up is because I know that that is a very, very common practice where multiple medications have to be given to the same patient over a period of time, like for example an anesthesia. And there are still providers out there from the old school where that was in fact acceptable. And thereís been an, you know, a misconception with that through the years. And I think this is a very good place to start. And I appreciate your willingness to relook at that. Joseph Perz: Thank you. Coordinator: Next question. Question: Thank you. My question is related to delivery of medication through other means like a transdermal or like through iontophoresis where in some cases youíll see individuals use the same syringe to draw up drug and then place it on a device like that to deliver the medication. Is there any recommendations related to that? Arjun Srinivasan: I think this gets back to the point that was actually just being raised is that there are considerations beyond blood borne pathogens here. And so, you see, clearly once youíve taken a needle and syringe thatís sterile, gone into a vial and youíve come out of the vial and you begin manipulating, that system is no longer sterile. It may not be contaminated with blood borne pathogens but thereís a risk that you can contaminate it, as the previous person was just pointing out, through manipulation and through putting it down, through having it touch the surface of a Ė something that might not be sterile. So I think that it would not be a good idea to then, you know, go back into that vial and reuse that needle and syringe, not from a blood borne pathogen standpoint but from the perspective that once you begin manipulating that setup it could be contaminated with whatever happens to be on the surfaces or on the hands of healthcare providers. Question Contíd: Thank you. Coordinator: Your next question. Question: Yes I would like to know if there are any updated recommendations for needle stick injuries aside from washing the site immediately and some kind of testing and also prophylactic meds? Arjun Srinivasan: Sir, can you repeat the question please? Question Contíd: Is there an updated recommendation as far as needle stick injuries aside from washing the site immediately, doing some HIV testing if needed and also giving the prophylactic meds? Is there an updated recommendation as far as thatís concerned, as far as needle stick injuries are concerned? Priti Patel: There are two MMWR reports that address this Ė with updated recommendations in terms of hepatitis C virus, hepatitis B virus and HIV exposures in healthcare settings. And so Iím not sure if youíre aware of those but those are both available on our Web site. Question Contíd: Okay, thank you. Coordinator: The last question; your line is open. Question: Hello. Yes I was wondering has alcohol been found to be effective enough against viruses when sanitizing multi-use vials and glucometers? And if not what is recommended to be used by the CDC at this point? Arjun Srinivasan: For disinfecting medical equipment you would need to use an EPA registered hospital disinfectant. And so alcohol in and of itself I donít think is licensed as an EPA registered disinfectant. So it does have some activity against the viruses but when youíre talking about cleaning a glucometers thatís a shared patient use item and it needs to be disinfected accordingly with an EPA registered disinfectant. Joseph Perz: The CDC recommendations have also advised that 1/100 solutions of bleach can be used. But again some of the glucometers themselves are not designed to withstand, you know, that particular agent. And as a reminder too that itís important to select a glucometer thatís not designed for individual patient use in their home but one thatís designed for institutional use. Alycia Downs: I want to thank our presenters again for providing our listeners with this information. And I want to thank our participants for joining us today. In case you didnít get the chance to ask a question please send an email to COCA. Thatís coca@cdc.gov. COCA@cdc.gov. The recording of this call and the transcript will be posted to the COCA Web site as they come to us. Our Web address is www.emergency.cdc.gov/coca. You have a year to obtain continuing education credits for this call. All continuing education credits for COCA conference calls are issued online through the CDC Training and Continuing Education online system, www2a.cdc.gov/tceonline. Again I want to thank our presenters for a wonderful call and I hope everyone has a great afternoon.
END |
|
|
|