Military
Hepatitis
History First known
existence of the
Hepatitis C
virus
Date of
Birth- WWII-
discovered by LB Seeff while
investigating
stored military blood
samples in 1977.
Samples examined were
from the 1942- 1944
outbreak of
Hepatitis among
troops that
received
yellow-fever
vaccine
stabilized with
human blood
Edwin Cohn,
John Oncley, and
colleagues at
Harvard
University
isolated the
gammaglobulin
fraction of
serum in 1944,
under contract
to the U.S.
Navy. Their
methods 6 and 9,
featuring a
cold-ethanol
fractionation
process, yielded
immune globulin
for
intramuscular
administration (IGIM,
“gamma
globulin”).
Joseph Stokes,
Jr., and John
Neefe reported
the utility of
IGIM in reducing
the incidence of
hepatitis A in
1945. Clinicians
primarily used
this drug to
prevent
or mitigate
measles, mumps,
hepatitis A, and
hepatitis B. (1,
2, 3, 6, 7, 9,
10, 46, 52-57)
IGIM
prevented
post-transfusion
hepatitis in
battle
casualties, if
given promptly.
(58) IGIM was
routinely
given to troops
assigned to
Korea or Vietnam
in the 1960s.
(9, 57, 59-62)
Korea & Vietnam
The Hepatitis
epidemic of 1942
caused by use of
batches of
yellow fever
vaccine
contaminated
with hepatitis
virus, coupled
with the
eruption of
200,000 cases of
viral hepatitis
between 1942 and
1945, identified
the disease as a
matter of prime
importance to
our Armed Forces
during World War
II (MD-IM3, p.
332). It became
evident during
these conflicts
that effective
methods to treat
or prevent
hepatitis in
soldiers were
urgently
required.

http://history.amedd.army.mil/booksdocs/vietnam/GenMedVN/ch18.html
May 01, 2007,
05:25:02 pm
Chapter 18
Hepatitis Page
431
J
oe
A. Dean, M.D.,
and Brigadier
General Andre J.
Ognibene, MC,
USA
VIETNAM
EXPERIENCE
Organized
study of the
large numbers of
troops afflicted
with hepatitis
was not
undertaken in
Vietnam;
attention was
focused on
prevention and
therapy. As
early as the
1940's, Stokes
and Neefe (1945)
reported that
epidemic icteric
hepatitis could
be either
prevented or
attenuated by
the parenteral
administration
of human serum
gamma globulin.
In 1964, a
program designed
to protect all
military
personnel
stationed in
Asia against
hepatitis was
instituted.
A
16-percent
solution of
human serum
gamma globulin
in a dose of
0.05 ml/lb was
used. The
gamma globulin
was prepared
from blood
donated in the
United States. A
significant
decrease in the
prevalence of
hepatitis during
that year as
compared to the
previous year
was seen in
preliminary
observations in
both Korea and
Vietnam.
However, close
examination of
monthly
hepatitis rates
revealed that
the decrease had
begun 4 months
before the gamma
globulin
prophylaxis
program was
initiated. Thus
it was
impossible to
determine
whether
--------------------------------------------------------------------------------
432
the
incidence of
icteric
hepatitis in
American troops
hospitalized in
Southeast Asia
was
significantly
affected by the
administration
of gamma
globulin from
the United
States (Conrad
1972).
[Update:
Process used to
make gamma
globulin didn't
work...1999-Safety
and availability
of
immunoglobulin
...potentially
transmissible
agents
Process used to
make human serum
gamma globulin
failed to rid
serum gamma
globulin of
blood borne
pathogens... like
hepatitis C.
Read]
With the
increasing
involvement in
Vietnam after
1965, national
stockpiles of
gamma globulin
were
significantly
depleted and a
reassessment of
the prophylactic
program was
necessary. The
dose of gamma
globulin
administered to
soldiers was
reduced to 5 ml
of a 16-percent
solution after
arrival
overseas, with a
second injection
5 months later
(DA Circ). It
was decided, in
1966, that only
persons under
high risk of
exposure to
infectious
hepatitis would
receive the
inoculations of
gamma globulin.
A continuing
incidence
greater than
five cases per
1,000 per year
in particular
units was
suggested as a
guideline for
this high risk
group.
No
significant
increases in the
incidence of
hepatitis during
the next year
were associated
with the
decreased
utilization and
dosage of gamma
globulin. In
Vietnam, the
case rates for
viral hepatitis
ranged between 4
and 10 per 1,000
troops per annum
(HOA). A
systematic study
of the policy of
prophylactic
gamma globulin
administration
in high risk
patients was
never
accomplished in
Vietnam.
However, a
large body of
data was
available from
the Korean era
(Conrad 1969).
Conrad (1972)
did a study of
all soldiers
arriving in
Korea through a
single airport.
Between May
1967 and August
1969,
107,803 troops
were given, upon
arrival, either
a 10-ml
injection
containing 2 ml,
5 ml, or 10 ml
of a 16-percent
human serum
gamma globulin
or a 10-ml
albumin-sucrose-potassium
glutamate
solution. A
second injection
of the same
material was
given to 65
percent of these
soldiers 5 to 7
months later.
Soldiers having
symptoms or
physical
findings of
hepatitis were
hospitalized and
examined. A
liver biopsy
specimen was
obtained fom 82
percent of the
patients.
Results showed
467 documented
cases of icteric
viral hepatitis
in the subjects
studied. The calculated
incidence was
5.67 cases per
1,000 among
the control
subjects, who
received the
albumin, while
among soldiers
given various
amounts of gamma
globulin it was
4.04 (2 ml
group), 3.39 (10
ml group), and
2.90 (5 ml
group) cases per
1,000.
Significant
protection was
provided to
those receiving
2 ml of gamma
globulin but
slightly less
than that which
was observed
with 5 ml. The
larger dose of
10 ml did not
produce a
further
reduction in the
incidence of
viral hepatitis.
In addition,
there was no
significant
difference
between the
incidence of
other infectious
diseases in the
gamma
globulin-protected
group and in the
control group.
Conrad also
compared the
hospital records
of patients who
received the 5-
or 10-ml dose of
gamma globulin
with those of
patients
injected with
placebo, to
determine
whether gamma
globulin
affected the
severity of the
illness. Again,
no significant
differences
appeared between
the groups. Since almost
none of the
patients studied
had had blood
transfusions, it
was believed
that most were
infected orally.
The
availability of
data showing
minimal
differences
between treated
and untreated
groups in mass
prophylaxis
reinforced the
policy in
Vietnam of
providing only 2
ml of gamma
globulin to
individuals in
whose units a
significant
epidemic
exposure was
manifest. There
is no evidence
that this policy
had any effect
on the incidence
or severity of
disease.
[Update:
1999,
Sterilants and
Disinfectants
Hepatitis C
Survives
Treatment with
Commercial
Sterilants and
Disinfectants
Applied and
Environmental
Microbiology, p.
4255-4260, Vol.
65, No.
90099-2240/99/$04.00+0]
Read
--------------------------------------------------------------------------------
433
As the number
of troops, and
consequently the
number of cases
of hepatitis,
increased and
the necessity
for air
evacuation of
these patients
from Vietnam
became apparent,
the prolonged
period of
treatment and
hospitalization
not only caused
a loss of duty
time but also
produced a
logistical
problem of
evacuation and
replacement. The
opening of the
6th Convalescent
Center at Cam
Ranh Bay,
Vietnam, on 16
May 1966,
provided a way
station to which
hepatitis
patients could
be evacuated for
convalescence.
However, the
prolonged
recovery phase
was still a
major factor
contributing to
the number of
man-days lost to
combat units.
In examining
the problem of
treating
hundreds of
patients with
infectious
hepatitis at the
6th Convalescent
Center, Repsher
and Freebern
(1969) were
impressed by the
benignity of the
clinical course
in most of the
patients, the
occur rence of
relapses despite
adherence to a
bed rest
regimen, and the
uneventful
clinical course
of patients who
engaged in
physical
activity
contrary to
advice. Based on
these
observations,
they performed a
pilot study on
the effect of
vigorous
reconditioning
on patients
whose liver
function tests
had not
completely
returned to
normal values.
The effect of
exercise on
recovery from
viral hepatitis
had been
reviewed earlier
by Chalmers et
al. (1955) and
Nefzger and
Chalmers (1963),
whose extensive
studies led to
the conclusion
that patients
allowed ad
libitum activity
improved just as
rapidly as those
kept on strict
bed rest. In
addition,
patients who
returned to
active physical
rehabilitation
as soon as the
results of their
liver function
tests were
relatively
normal were
found to have an
uncomplicated
convalescence
similar to that
of patients
returned to duty
much more
gradually.
Nelson and
coworkers (1954)
had reexamined,
2 to 3 years
after onset of
disease,
patients who had
had ad libitum
exercise. Their
studies included
hepatic biopsies
in 40 of the 80
patients, all of
which showed no
evidence of
residual liver
disease.
Furthermore,
Repsher and
Freebern's
review of
existing
literature
indicated an
absence of
controlled or
prospective
studies
demonstrating
any benefit from
the traditional
enforced bed
rest regimen.
Repsher
and Freebern
(1969) then
undertook a
prospective
study of 398
American
servicemen at
the 6th
Convalescent
Center.
Inclusion in the
study required
elevations of
serum bilirubin
concentration
and SGOT.
Patients were
examined to
preclude the
presence of
malaria,
infectious
mononucleosis,
pneumonia, or
other illnesses.
They were
required to have
been
asymptomatic
with return of
appetite for
less than 5 days
despite the
persistence of
abnormal liver
function.
Evidence of
previous
hepatitis or
history of blood
transfusion in
the preceding
year excluded
patients from
the study.
Patients were
divided randomly
into rest and
exercise groups.
The rest group's
activity was
restricted to a
100-yard walk to
the messhall and
a walk to the
theater or post
exchange; they
were otherwise
confined to the
ward. The
exercise group
participated in
a 1-hour session
of calisthenics
6 mornings a
week, including
a 1-mile run
and, for 4
afternoons a
week, a 2-hour
work detail
filling
sandbags,
painting
buildings, and
constructing
bunkers. This
group also
participated in
supervised
athletics
including
softball,
swimming,
volleyball, and
basketball.
During the
period of study,
all groups were
under the direct
observation of
the assigned
physicians.
--------------------------------------------------------------------------------
434
Comparison of
these groups
showed no
difference in
duration of
illness. In
one-third of the
cases, the SGOT
was still
elevated when
the serum
bilirubin had
returned to
normal, a
situation no
more frequent in
the exercise
group than in
the rest group.
While recovery
time was
unchanged in the
two groups, the
time to return
to duty was
shorter for the
exercise group.
The exercise
group was shown
to be fit for
return to combat
duty immediately
on completion of
hospitalization.
The rest group,
however,
required
conditioning and
observation
before discharge
and appropriate
disposition
could be made.
As a result of
this study,
individuals
recovered from
hepatitis were
returned to
combat duty
earlier than had
been possible in
the past.
Repsher and
Freebern
cautioned
against making
generalizations
about infectious
hepatitis in all
adults from
studies of the
disease in this
military
population of
otherwise
healthy young
men.
Furthermore, the
origin of the
disease may
differ in
different parts
of the world.
They also warned
against applying
their findings
to Type B
hepatitis,
inasmuch as
presumably their
cases were
caused by Type A
virus.
The studies of
Krugman, Ward,
and Giles (1962)
indicated that
in most cases
virus is
excreted from
about 16 days
before icterus
to about 8 days
after its
appearance.
Based on this
information, no
attempt was made
to separate the
exer cise group
from the other
patients at the
6th Convalescent
Center. Most
patients had
been
hospitalized
primarily at an
evacuation or
field hospital
before transfer
to the
convalescent
center, with an
average of 8
days' delay
before arrival
there. Normal
hygiene was
maintained but
isolation
procedures for
hepatitis
patients were
not practiced.
They shared
common dining
facilities with
the staff and
with other
patients. During
the 6 months of
the study, none
of the patient
contacts
developed
hepatitis; only
one case was
identified in a
staff member in
the year that
followed, but it
could be
attributed to
eating in a
local village.
Thus, this study
was responsible
for simplifying
hospital care
for hepatitis
patients in
addition to
significantly
reducing combat
man-days lost.
Returning the
individual to
his parent unit
reduced the need
for
out-of-country
evacuation and
replacement from
the continental
United States.
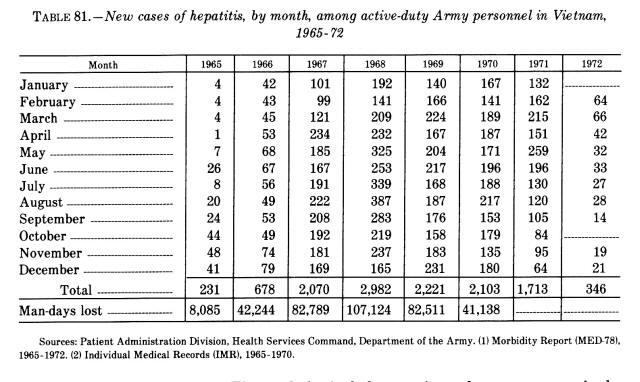
Table 81 lists
the number of
cases of
hepatitis, by
month, in
Vietnam for
1965-72 and the
numbers of
noneffective
days for
1965-70. While
the number of
cases per year
remained fairly
constant, the
noneffective
days decreased
by 65,986
between 1968 and
1970. The
average time
lost from duty
per individual
thus decreased
from 35.7 days
to 18.6 days
during that
period.
While an
exercise program
for the patient
with
uncomplicated
hepatitis was
shown to be
appropriate in a
combat theater,
considerable
concern arose
regarding those
patients who
might have
chronic active
hepatitis.
Studies by Anand,
Tamburo, and
Leevy (1971) had
shown some
detrimental
effect of
exercise on
hepatic function
in patients with
chronic active
hepatitis. At
the 6th
Convalescent
Center, Jolson
and Blailock
(1970) studied
26 patients with
a clinical
diagnosis of
viral hepatitis,
randomly
selected for
aspiration liver
biopsy by the
Menghini
technique. Six
of these
patients were
noted to have
some increase in
portal collagen
and minimal
fibrous
interconnecting
bridging. Three
of the six had
evidence of
focal, piecemeal
necrosis at the
limiting plate
compatible with
chronic active
hepatitis.
Followup of
these three
patients was
obtained with
--------------------------------------------------------------------------------
435
TABLE
81.-New cases of
hepatitis, by
month, among
active-duty Army
personnel in
Vietnam, 1965-72
biopsies 30
to 90 days
later. The
pathological
changes in each
case
progressively
decreased in
severity as
fibrous
interportal
bands
disappeared.
Results were
inconclusive,
though they
suggested that
additional
studies on
larger numbers
of patients
might be
considered.
The
success of the
6th Convalescent
Center's
programs in
returning
hepatitis
patients to duty
resulted in
publication of
an official fact
sheet on
management and
evacuation
policy by Col.
Philip J. Noel,
Jr., MC, USARV
(U.S. Army,
Vietnam) surgeon
(1970). The text
of the fact
sheet follows:
The projected
possibility of a
shortage of
convalescent
beds has not
materialized.
Therefore, the
following
management
practices for
viral hepatitis
patients are
being
established.
All
patients with
viral hepatitis
will be admitted
to an acute
treatment
facility. When
subjective
symptomatology
improves, the
patient will be
transferred to
the 6th
Convalescent
Center.
Patients
contracting
viral hepatitis
with over ten
months
in-country will
be evacuated
directly from
the acute
treatment
facility to
CONUS. Their
clinical status
should be stable
prior to
disposition.
Those patients
transferred to
the 6th
Convalescent
Center will
undergo a
program of
treatment and
graded physical
exercise and
reconditioning.
This program
will allow most
of the affected
individuals to
be returned to
full duty.
Those patients
whose clinical
states do not
warrant return
to full duty
within the
limits of the
established
evacuation
policies will be
returned to
CONUS.
The important
point is the
requirement for
a physical
activity
program.
However, with
American
withdrawal and
the increase in
hepatitis
related to drug
abuse,
(definitive
conclusions
about the
long-term
followup of
patients treated
with daily
exercise could
not be reached.
Many questions
remain for
future study in
large troop
populations with
hepatitis,
especially if
therapy
continues to
include early
ambulation,
exercise, and
early return to
duty.
It was indeed
fortunate that
the major
complications of
hepatitis were
infrequently
seen in Vietnam.
Although a
limited number
of patients
developed
fulminant
hepatitis, as a
general rule
most patients
had
uncomplicated
--------------------------------------------------------------------------------
436
recoveries
without
significant
sequelae.
Problems with
hepatitis in
drug abusers
will be
discussed in
volume III of
this series on
internal
medicine in
Vietnam.
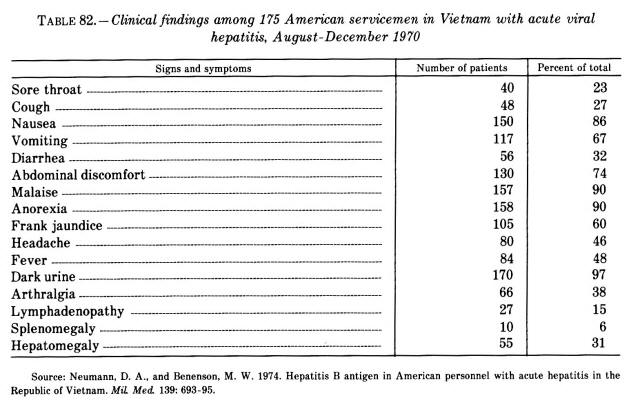
Following the
discovery of
hepatitis B
antigen, viral
hepatitis could
be divided into
two major groups
based on the
antigen's
presence or
absence. To
determine the
importance of
HBS Ag positive
hepatitis in
Vietnam, Neumann
and Benenson
(1974) studied
patients
admitted to four
U.S. military
hospitals with a
diagnosis of
acute viral
hepatitis. From
August to
December 1970,
175 American
servicemen with
acute viral
hepatitis were
studied and
information was
gathered on
possible
exposure to
other persons
with hepatitis
and other
epidemiological
variables. HBS
Ag was detected
in the serum of
71 of these
soldiers. There
appeared to be
no relationship
between the
presence of the
antigen and
race, sex,
location, eating
habits, drug
use, or contact
with other
hepatitis cases.
The signs and
symptoms of
disease among
all patients are
noted in table
82.
The
epidemiology of
Type B hepatitis
was studied only
late in the
conflict and
includes Thai
and Cambodian
population
samples as well
as American.
Table 83
demonstrates the
prevalence of
antigenic
markers of
hepatitis B
subgroups in
varied
populations. The
antigenic
subtypes of
Americans
stationed in
Southeast Asia
were unlike
those of the
indigenous
populations and
those of
Americans in the
United States (Snitbhan
et al. 1975).
The adr subtype,
present in 85
percent of
asymptomatic
Asians, is noted
in only 2.5
percent of
Americans in the
United States.
However, it is
found in 40
percent of
American
asymptomatic
carriers in
Asia. Such
differences
indicate that
Americans
acquire HBS Ag
of subtype adr
in Asia.
Subtypes are
region-dependent
and not solely
related to
national origin.
The presence of
adr in Americans
with hepatitis
suggests
transmission
from the local
population and
the frequency of
ayw confirms
passage of
infection from
one American to
another. The
future study of
subtypes can
offer an
effective
epidemiological
tool in review
of large
populations.
Epidemics
related to Type
A hepatitis were
documented in
units in Vietnam
(Kunkel 1967).
An episode of 71
cases of viral
hepatitis among
1st Infantry
Division
personnel
occurred between
3 April and 1
June 1967, while
they were
engaged in
Operation
JUNCTION CITY in
War Zone C near
the Cambodian
border. All of
the afflicted
individuals had
been in the
field during the
estimated time
of the exposure;
92 percent were
found to have
been in one of
the villages in
the operations
area, and 94
percent had been
assigned duties
at a single
bridge site.
Further
investigation
incriminated
nonpotable ice
supplies.
Waterborne Type
A hepatitis was
well documented
as far back as
the 1930's and
1940's; however,
it did not
become part of
everyday
epidemiological
consideration
until the Delhi
epidemic of
1955-56, which
involved 29,300
cases (Mosley
1972). Scattered
reports of
epidemic
outbreaks most
likely related
to iceborne or
waterborne
routes were
characteristic
of the Vietnam
experience.
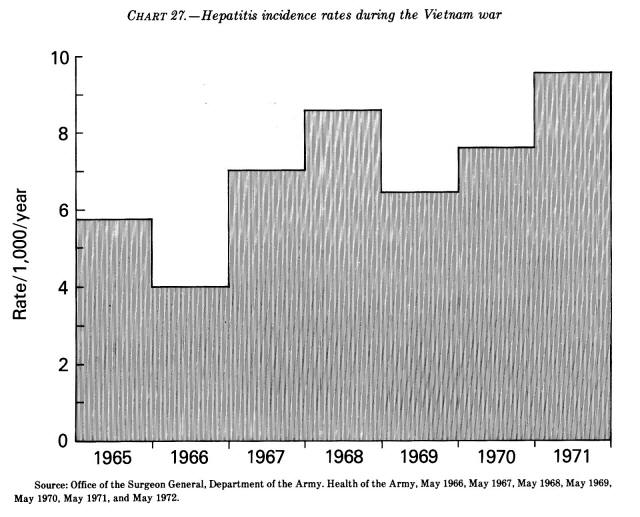
An
analysis of
hepatitis rates
(chart 27) for
the Vietnam war
reflects three
major phases.
The first years,
when activities
were limited,
were
characterized by
a low incidence
rate. This was
soon followed by
rising rates as
more troops
became exposed
to the
environment and
as established
principles of
hygiene and
discipline were
less effectively
enforced. In
1968-69,
however,
personal hygiene
--------------------------------------------------------------------------------
437
TABLE
82.-Clinical
findings among
175 American
servicemen in
Vietnam with
acute viral
hepatitis,
August-December
1970
CHART
27.-Hepatitis
incidence rates
during the
Vietnam war
--------------------------------------------------------------------------------
438
was
emphasized and
unit awareness
was aroused.
This was
followed by a
drop in the
incidence rate.
However, as the
problem of drug
abuse developed,
rates again
rose. Studies at
that time
(Neumann and
Benenson 1974)
revealed 41
percent of the
patients were
afflicted with
type B
hepatitis; this
was the first
time such data
were available
in Vietnam and
reflected a
shift in the
epidemiology of
the disease.
With U.S.
withdrawal,
further study
was aborted.
Related
link:
-
Blood, Plasma,
and Related
Programs in the
Korean War
A plasma
program was
also
developed
which later
had to be
discontinued
because of
the risk of
serum
hepatitis
associated
with plasma
infusions
-
Human Serum
Gamma
Globulin
A
16-percent
solution of
human serum
gamma globulin
in a dose of
0.05 ml/lb was
used. The
gamma
globulin was
prepared
from blood
donated in
the United
States
prisons and
processed in
Canada.
- 1969
New York
Times-
many people
sickened and
some died in
an extended
series of
drug tests
and blood
plasma
experiments
- 1990
Follow-up
More Than 40
Years Later
Hepatitis C
Epidemiology in
Military and
Veteran
Populations:
Proceedings of
the Second
Biennial
Conference,
March 7, 1990
(1991)
Institute of
Medicine- Yellow
Fever
Vaccine-Associated
Hepatitis
Epidemic During
World War II:
- 1995
Philadelphia
Inquirer
“On the
Trail of
Tainted
Blood"-
provides an
in-depth
report of
our
Governments
knowledge of
Hepatitis
transmission....
Experiments
with human
volunteers
from the
military,
prisons and
state
hospitals
were
abandoned...plasma-induced
hepatitis
- 1999,
Sterilants and
Disinfectants
Hepatitis C
Survives
Treatment with
Commercial
Sterilants and
Disinfectants
Applied and
Environmental
Microbiology, p.
4255-4260, Vol.
65, No.
90099-2240/99/$04.00+0]
-
1997 DoD
Jetgun Report- Vaccines in the Military Report- Vaccines in the Military-
Department of Defense- Wide review of Vaccine Policies and Procedures...Jet
injector nozzles were frequently contaminated with blood
-
Hepatitis C Epidemic Blood
Industry TOC