Problems Persist With Red Cross Blood Services
Jessica Kourkounis for The New York Times
 In 2004, auditors found that the Red Cross’s operation in Philadelphia failed to recall some 600 units of blood collected using improper methods. In 2004, auditors found that the Red Cross’s operation in Philadelphia failed to recall some 600 units of blood collected using improper methods.
By
STEPHANIE STROMPublished: July 17,
2008
For 15 years, the
American Red Cross has been under a
federal court order to improve the way it
collects and processes blood. Yet, despite
$21 million in fines since 2003 and repeated
promises to follow procedures intended to
ensure the safety of the nation’s blood
supply, it continues to fall short.
Quality
control has been a problem at
the Red Cross.
The situation has proved so frustrating
that in January the commissioner of food and
drugs attended a Red Cross board meeting — a
first for a commissioner — and warned
members that they could face criminal
charges for their continued failure to bring
about compliance, according to three Red
Cross officials who attended the meeting and
requested anonymity because Red Cross policy
prohibits public discussion of its meetings
with regulators.
“If fear is a motivator, we’re happy to
help out in that way,” said Eric M.
Blumberg, deputy general counsel at the
Food and Drug Administration, though he
declined to confirm what the commissioner,
Andrew C. von Eschenbach, said at the
meeting.
Some critics, including former Red Cross
executives, have even suggested breaking off
the blood services operations from the rest
of the organization, as the Canadian Red
Cross did a decade ago.
The problems, described in more than a
dozen publicly available F.D.A. reports —
some of which cite hundreds of lapses —
include shortcomings in screening donors for
possible exposure to diseases; failures to
spend enough time swabbing arms before
inserting needles; failures to test for
syphilis; and failures to discard
deficient blood.
In some cases, the lapses have put the
recipients of blood at risk for diseases
like
hepatitis,
malaria and syphilis. But according to
the food and drug agency, the Red Cross has
repeatedly failed to investigate the results
of its mistakes, meaning there is no
reliable record of whether recipients were
harmed by the blood it collected.
The Red Cross, which controls 43 percent
of the nation’s blood supply, agrees that it
has had quality-control problems and is
working to fix them. Both its officials and
the drug agency point out that none of the
identified problems involve the most serious
category of infractions. For instance, the
Red Cross does a good job of testing for
H.I.V. and
hepatitis B, officials on all sides
agree. And in general, Red Cross blood is
regarded as some of the safest in the world.
Still, the drug agency says, the problems
that remain in screening donors and
following protocols for collection add
unnecessary risk to blood transfusions,
almost five million of which were done in
2007, according to the National Heart, Lung
and Blood Institute.
“This is a critical piece of the public
health infrastructure,” Mary A. Malarkey,
director of the Office of Compliance and
Biologics Quality at the drug agency, said
in an interview. “I know it’s difficult to
get so many people trained and properly
supervised, but it has to be done.”
This week, the agency sent the Red Cross
the results of yet another recent
investigation that makes Ms. Malarkey’s
point: From December 2006 to April 2008, the
Red Cross distributed more than 200 blood
products that it had already identified as
problematic, according to the investigation
report.
A Troubled History
While many Americans see the Red Cross as
the ubiquitous organization that responds to
disasters big and small, its disaster-relief
operation, which spends $400 million to $500
million annually, is small compared with its
blood business, which generated $2.1 billion
in revenue in the fiscal year that ended in
June 2007.
In fact, the Red Cross is the world’s
largest single steward of blood, more than
twice the size of the second-largest known
blood collection operation. The rest of the
world’s blood supply is controlled by dozens
of smaller organizations, only three of
which have ever been under F.D.A.-requested
consent decree.
After years of quiet complaints about the
Red Cross’s blood business, the F.D.A.
reluctantly decided to go public with its
concerns in 1993, obtaining a consent decree
that required the Red Cross to strengthen
quality control and training and improve its
ability to identify, investigate and record
problems.
“It was one of the hardest things I did
as commissioner,” said Dr.
David A. Kessler, the F.D.A.
commissioner from 1990 to 1997. Dr. Kessler
said he had agonized that the move would
cause undue alarm.
The news media, however, barely made note
of it.
Fifteen years later, that consent decree,
toughened in 2003 to allow the F.D.A. to
impose fines for failing to properly
identify, handle and report quality control
problems, has produced only modest
improvements, food and drug officials said.
“Leaving aside who’s at fault here, it’s
not working,” said Dr. Kessler, now a
professor of pediatric medicine at the
University of California, San Francisco.
“Whether it’s that the American Red Cross
just doesn’t get it, whether it’s that the
relationship between the regulator and
regulated is beyond the point of repair is
immaterial. It’s just not working.”
Dr. Kessler said Congress should
intervene at this point. (Page 2 of 3)
Dr.
Bernadine Healy, the former chief
executive of the Red Cross who made
repairing the organization’s blood
operations a paramount goal, said the best
solution might be to spin off the Red
Cross’s blood services.

Jessica Kourkounis for The
New York Times
Despite a
federal court order to improve,
the Red Cross has had problems
for years ensuring the safety of
the blood it collects and
processes.

Jessica Kourkounis for The
New York Times
“Two-thirds of the revenue base of the
Red Cross is blood, yet the Red Cross is run
by people who think of it as primarily a
disaster-relief organization, relegating
blood to stepchild status,” Dr. Healy said.
“When is the last time you saw a Red Cross
fund-raising appeal for money to make the
blood supply safer or support its blood
research?”
Dr. Healy said she tried to start such a
fund-raising program when she ran the Red
Cross, but met internal resistance to it.
The Red Cross has toyed with selling off
its blood operations, or otherwise
decoupling them from its disaster work, but
has never done so, in part because of a
belief that the billions in revenue from
blood has subsidized its disaster
operations. But its financial systems are so
antiquated that no one really knows.
“I can’t tell you that for sure because I
can’t find it out,” said Kevin M. Brown, the
Red Cross’s chief operating officer. “I wish
I could.”
Mr. Brown noted, however, that the blood
business was an integral part of the Red
Cross. “It is consistent with our overall
mission, which is saving lives,” he said.
“Having an ample and safe blood supply is
critical to that mission.”
Failing to Act
The frustrations of dealing with the Red
Cross are illustrated by the story of
Michelle Hoyte, a whistle-blower who was
first ignored, then dismissed.
Ms. Hoyte led a team of auditors who
conducted a routine visit to the Red Cross
blood services operation in Philadelphia in
2004. The team discovered that the facility,
with the approval of a senior executive at
the national headquarters in Washington, had
decided not to recall some 600 units of
blood collected using improper methods.
Such mistakes must be reported in writing
to the F.D.A. within 15 days of detection,
and the blood must be recalled. But Ms.
Hoyte spent six months pleading with various
supervisors to report the problem, first
identified on Dec 18, 2003. Then she was
fired.
“It wasn’t just that I thought it was the
right thing for them to do; they are
required to tell the F.D.A. under the terms
of the consent decree,” Ms. Hoyte, who
worked for the F.D.A. before joining the Red
Cross, said in an interview. “They didn’t
want to hear it.”
Ms. Hoyte, who unsuccessfully sued the
Red Cross for wrongful termination, had
received “excellent performance appraisals,”
according to the lawsuit, and received a
bonus and merit raise in the two years
before her firing.
The Red Cross contends that her dismissal
had nothing to do with her insistence on
abiding by the court order. It said in court
papers that she had been warned of
shortcomings in her performance.
The Red Cross also defended its handling
of the episode. “They followed the process
and did what they should have done,” said
Eva Quinley, the senior vice president for
quality and regulatory affairs at the Red
Cross.
But the Red Cross did not recall the
components produced from that blood until
Feb. 23, 2005, 14 months after the problem
was discovered, according to an F.D.A.
report. By then, those components would have
been used or discarded, and whether they
caused any problems for patients is unknown.
Determining how often, if ever, blood
supplied by the Red Cross has been
responsible for serious health problems is
difficult. F.D.A. documents rarely spell out
the consequences of the failures they
catalogue, a reflection, to some degree, of
the agency’s concern about alarming the
public. But often they simply do not know.
“Patients who get blood transfusions tend to
be pretty sick,” Dr. Healy said. “If they
spike a
fever post-transfusion, no one is likely
to suspect that the blood caused it.”
Various records of F.D.A. inspections and
correspondence with the Red Cross highlight
poor follow-up, including falsified records.
On Nov. 19, 2001, for example, a patient
receiving blood bought from the Red Cross’s
greater Chesapeake and Potomac region, which
serves the Washington area, died of
hepatitis, according to an F.D.A. report.
The agency concluded that the Red Cross had
failed to perform a thorough investigation.
Furthermore, the drug agency found that
the Red Cross had failed to investigate 134
cases of suspected post-transfusion
hepatitis that occurred across all its
regions from January 2000 to June 2002.
Ms. Quinley said procedures had been
changed since then in an effort to ensure
that such cases would be investigated.
A Fractured System
(Page 3 of 3)
Until 1991, Red
Cross blood
operations were
largely controlled
by its regional
chapters, which
operated 53 blood
centers in vastly
different and often
idiosyncratic ways.
That year,
Elizabeth Dole,
then chief executive
of the Red Cross,
announced a sweeping
overhaul that
wrested control of
the blood operations
from the chapters
and reorganized them
into 10 regions,
which were expected
to adhere to a
uniform set of
standards and
procedures.
That event is
still referred to
among many at the
Red Cross as “the
Divorce,” a measure
of the
organization’s
entrenched culture.
While Mrs. Dole
won praise for
taking a bold step
to address a long
history of sloppy
testing and record
keeping that raised
concerns among
regulators and the
public about blood
being potentially
contaminated with
H.I.V., chapters and
their staff and
volunteers saw it as
an effort by the
national
headquarters to
control the vast
amount of money the
blood services
generate.
That legacy
persists.
“We have never
truly moved away
from independence to
national, central
standards,” said J.
Chris Hrouda,
executive vice
president and a
20-year veteran of
the Red Cross’s
biomedical services,
as the blood
operations are
known.
Nor did anyone
anticipate the cost
and difficulty of
the reorganization,
current and former
executives said. At
first the project
was budgeted at $120
million, but the
cost of developing a
centralized database
has run to at least
$1 billion so far,
according to
estimates by former
executives. The
database would make
it easier to track
down flawed blood
components and to
flag donors who have
been previously
screened out because
of diseases or
travel to places
where malaria is
common.
“There is no
system to meet our
needs,” Mr. Hrouda
said. “We are six
times the size of
the next-largest
blood operations,
and clearly that’s a
hindrance.”
A small company
in Paris, Mak-System
International Group,
is working to create
such a system, but
Mr. Hrouda had no
estimate of when it
would be up and
running.
Thus, the Red
Cross’s current
blood operations, 36
regions grouped into
seven divisions
served by five
testing
laboratories, are
still controlled by
different systems
that cannot easily
“talk” to one
another.
In the meantime,
the Red Cross has
incorporated
technology intended
to help it prevent
mistakes when blood
is collected.
The most frequent
errors cited by
F.D.A. investigators
involve failing to
ask donors questions
that would reveal
their ineligibility
to give blood. For
instance, an
interviewer forgets
to ask a donor
whether he has
traveled in an area
where malaria is a
problem. So
increasingly, donors
fill out online
questionnaires,
which helps ensure
that all required
questions are
answered.
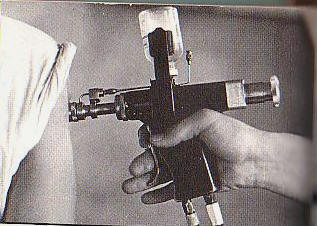
Blood collection
is also error prone,
governed as it is by
strictly prescribed
procedures. After
phlebotomists locate
a vein, they must
scrub a
3-inch-by-3-inch
area with antiseptic
soap for 30 seconds,
then use an
antiseptic swab and,
starting at the
point where they
will insert the
needle, work
outwards in
concentric circles.
They must then allow
the area to dry for
precisely 30 seconds
before inserting the
needle.
To improve that
process, Red Cross
phlebotomists
recently began
wearing electronic
devices that time
each of those steps.
The organization
is also improving
oversight on the
mobile units used to
collect roughly 80
percent of the blood
it processes by
assigning full-time
supervisors.
Such measures,
however, are
undercut by high
turnover among
employees, who are
paid little better
than minimum wage,
former executives
say.
Mr. Hrouda said
there was no plan to
address high
turnover. “We think
we’re able to
recruit people at
the wages we pay and
are good at training
them,” he said.
The F.D.A.,
however, sees the
main problem
differently. “Size
is no longer an
excuse,” said Mr.
Blumberg, the
agency’s deputy
general counsel.
Ms. Malarkey, of
the F.D.A.’s Office
of Compliance and
Biologics Quality,
said: “Right now,
the biggest issue
confronting the Red
Cross is what we
refer to as their
problem management.
They have standard
operating procedures
by which they should
be able to
investigate,
evaluate, correct
and control to
prevent recurrence
of the issues we
have identified
again and again, but
they have a lot of
difficulty
implementing those
procedures and,
frankly, in having
people follow them.”
Ms. Malarkey said
a recent “adverse
determination
letter,” the process
through which the
F.D.A. informs the
Red Cross of
violations it has
identified and
demands payment of
fines, illustrated
her point.
In that letter,
dated Feb. 8, the
drug agency listed
113 “events”
involving 4,094
flawed blood
components that were
recalled by 15 of
the Red Cross’s 36
regions. The recalls
occurred largely
from April 15, 2003,
to April 15, 2006.
(It is not uncommon
for letters to list
hundreds of
infractions — one
2005 letter
identified more than
22,000 flawed blood
components that were
recalled — and
recalls do not mean
every blood product
is returned.)
“We are not
seeing what we were
seeing in the late
1980s and early
1990s, where
unsuitable blood was
routinely being
released,” Ms.
Malarkey said, “but
they still need to
make more progress,
and we would like to
see that progress
made quickly.”
http://www.nytimes.com/2008/07/17/us/17cross.html?pagewanted=3&_r=2&hp&adxnnlx=1216289519-PakcZC8LgRzjzM9JHjlj9g
Related:
Times Topics: American Red Cross
Enlarge This Image

Jessica Kourkounis for The
New York Times
http://topics.nytimes.com/top/reference/timestopics/organizations/a/american_red_cross/index.html
|