|
|
||||||||||||||||||||||||||||||||
|
|
|
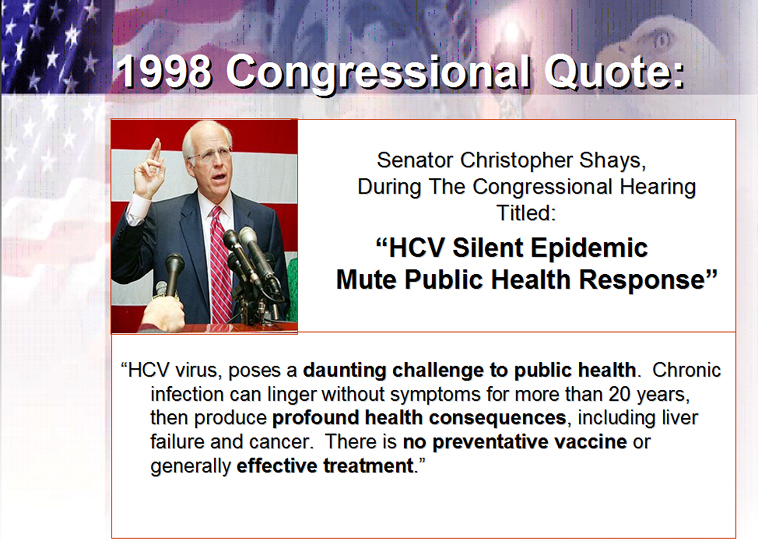
Natural History of HCV Hepatitis C is often asymptomatic. Most symptoms begin only when irreversible liver damage (cirrhosis) is established. The best outcomes for HCV patients depend upon early recognition of the infection. Any person with risk factors should be screened for HCV. Multiple studies have shown that earlier treatment of patients who have chronic liver disease associated with hepatitis C results in improved outcomes. Chronic infection with HCV is an epidemic within the United States. A majority of patients who acquire hepatitis C will progress to some form of chronic liver disease. Recent evidence published in the New England Journal of Medicine indicates some patients may have a long course in which the disease does not causes significant damage to the liver. However, it is difficult to identify those patients since their clinical characteristics are unknown. There are no blood or radiologic tests which identify this group of HCV patients. Most patients who acquire HCV infection are not aware that they have become infected. Acute infection with HCV is usually associated with flu like symptoms and not jaundice (turning yellow). As a result, patients may have the infection for years before being identified. Most patients are identified during routine physical exam or blood donations. Abnormal liver function tests are identified during these evaluations. When abnormal liver function tests or a history of risk factors are identified, further testing is recommended. Once the infection has been established, the liver experiences inflammation which over 20 years may result in cirrhosis. It is thought that 85 % patients infected with HCV will develop some form of chronic inflammation of the liver. Of these patients, about 20 % will develop cirrhosis of the liver after about 20 years of infection. Some patient populations seem to tolerate the infection better than others. These patients are under investigation to identify the means by which this is accomplished. The primary goal for patients with HCV is early institution of therapy to prevent the development of cirrhosis. Once cirrhosis is present, the response rates for treatment decrease significantly. In addition, the possibilities of developing complications from cirrhosis (such as hepatocellular carcinoma and portal hypertension) increase rapidly. Patients with Hepatitis C infection may have normal, fluctuating or persistently elevated ALT levels. It is important that these liver function test abnormalities be present for at least 6 months. However, if an individual has recently had been identified as having elevated liver function test, and has one or more of the above risk factors, an immediate test for the Hepatitis C antibody test (EIA) is appropriate. Hepatitis C is a heterogeneous infection. Its interrelationship with the human immune system is variable and difficult to correlate. However, some trends have been identified. In some patients serious liver disease may occur within the first several years. However, in most patients chronic liver disease requires infection for 20 to 30 years. When acquired in older age, the disease may progress more rapidly. Ingestion of alcohol has been clearly associated with an increased rate of hepatic inflammation. HCV patients who drink often have an acceleration of their disease. Associated Diseases Hepatitis C is thought to be associate with multiple other diseases: Lichen
planus.
The most common presentation of
hepatitis C is a patient with no complaints. Many patients, especially
when questioned closely, report a history of fatigue and malaise.
Intermittent right upper quadrant abdominal pain may also be present.
However, the typical patient with
hepatitis C will be asymptomatic and have normal, intermittently elevated,
or persistently elevated liver function test.
The primary problem for patients with
HCV and their physicians is communication regarding possible risk factors
for acquisition of the HCV virus. If you have a history of any of the risk
factors, please contact your physician.
Diagnosis of Hepatitis C
The initial test for hepatitis C is the
enzyme-linked immunoassay. This is also known as the enzyme immunoassay (EIA).
This test looks for the antibody to HCV in the blood. Over the past 10
years three generations of EIA antibody tests for hepatitis C has been
developed. The most commonly used today, EIA 3, is 95 percent specific and
sensitive for hepatitis C. However, this test, even when positive, needs
to be confirmed with a polymerase chain reaction (PCR)
to evaluate the presence of HCV virus. If the PCR is positive, further
blood testing for the viral load (amount of virus in one milliliter of
serum) and the genotype (type of HCV
present) can be performed. |
|